Age-Related Macular Degeneration (AMD)
Definition
Age-related macular degeneration (AMD) is a common condition affecting people age 50 years and older. The condition may be associated with central vision loss such as loss of the ability to read, to drive a car, or see someone’s face if it progresses to more advanced stages.
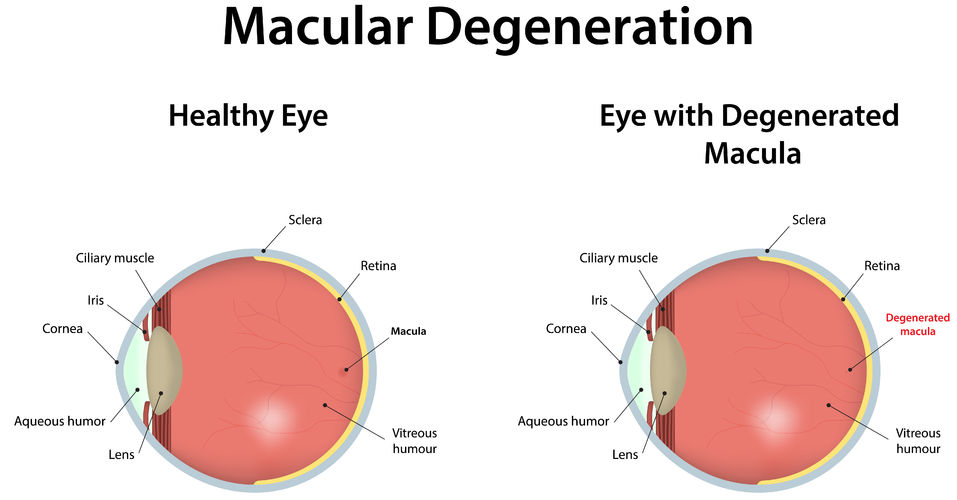
The macula refers to the central portion of the retina. The retina is similar to film inside a camera. The image one sees is focused by the cornea and lens of the eye and then cast upon the center of the retina (macula.) Many people with AMD have no visual symptoms and may retain normal 20/20 vision indefinitely. A relatively small percentage of people with AMD will lose central vision and the ability to read and drive a car. Although AMD can cause central vision loss, it does not typically lead to complete blindness.
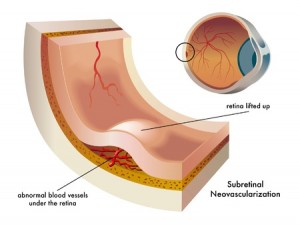
There are two major types of AMD, a “dry” (non-neovascular) and a “wet” (neovascular) form. The dry form is the early stage. It is the most common form of AMD. There is usually little or no vision loss during this stage although there are exceptions with some people having significant vision loss from more advanced “dry” degeneration. The wet form is a late stage of the condition and affects about 10 percent of all people with the condition. Wet AMD accounts for the majority of central vision loss due to AMD. The wet type implies leakage and bleeding in the macula due to abnormal blood vessels known as choroidal neovascularization. These abnormal blood vessels start to grow beneath the center of the macula and, as they grow, they leak fluid or blood and cause central vision loss with blurring and distortion of vision. Untreated, these abnormal blood vessels typically will grow relatively large and eventually cause scarring with permanent and often severe central vision loss.
The dry form of AMD is characterized by drusen. These are little yellow deposits that the doctor sees when looking at the macula on clinical examination. Drusen are the hallmark of AMD. Most people with drusen alone do not have significant visual changes or vision loss. A minority of people with dry AMD will advance to central vision loss due to geographic atrophy which is the loss of pigment layer under the macula. Unfortunately, there is no treatment or cure for geographic atrophy and the associated vision loss.
New treatments are in evolution for wet AMD and these treatments aim to halt the growth and leakiness of choroidal neovascularization. Injection therapies are the mainstays of treatment of wet AMD.
Causes and Associations
There are no known specific causes of AMD. It is a degenerative condition that occurs over time. It is typically found in people ages 50 years or more, although drusen sometimes can be seen in younger people. There tends to be familial associations, although just because a family member or blood relative has AMD does not destine someone else in the family to have it as well. Over time, the macula accumulates drusen and pigment changes, and if choroidal neovascularization or geographic atrophy is avoided, then vision tends to remain good. Progression to advanced AMD such as with the development of geographic atrophy or choroidal neovascularization (wet AMD) will result in central vision loss.
There are risk factors for people with AMD that may be modifiable or controllable. These include smoking, poor nutritional intake, and high blood pressure.
Symptoms
Many people with dry AMD have no visual symptoms at all. Some people, however, will require more light to read, have difficulty adjusting between dark and light conditions, or notice mild blurring of vision. Occasionally, significant loss of central vision can occur. Vision loss associated with dry AMD is usually gradual or slow. Because AMD affects the macula, the symptoms are typically related to central vision tasks such as reading or driving. Peripheral vision is typically not affected.
People with wet AMD often have more rapidly progressive loss of central vision, typically over weeks or months. Visual distortion is a common symptom of this stage. Occasionally, people may not be aware of these visual changes because the other eye may see well. Therefore, it is important to test vision in each eye separately by covering one eye at a time when checking vision.
An Amsler grid is a checkered pattern with a central dot in the middle of the pattern. It is a self-monitoring tool that allows people to check their vision one eye at a time to monitor for blurring or distortion that may signify the conversion from dry to wet AMD. People with AMD progression may notice changes on the Amsler grid, and if this occurs, they should contact their ophthalmologist promptly.
Evaluation
Complete and comprehensive ophthalmic examination is important in the assessment of AMD. People will receive vision testing, eye drops to dilate pupils, and a complete examination of the front and back of the eye. Pupillary dilation may create near vision blurring, and therefore, it is often best if a driver accompanies the patient, although it is not absolutely required.
People with AMD may have several types of tests to assess the disease. People may undergo color photography of the macula to document drusen, pigment changes, and other characteristics of AMD.
Fluorescein Angiography is a commonly used, office-based diagnostic test that can aide in determining the extent of macular degeneration and help distinguish between the dry and wet forms of the condition. Fluorescein angiography is performed by injecting sodium fluorescein dye into a peripheral vein with a small needle. This dye then goes through the blood vessels of the body and eyes. Choroidal neovasculation in the macula can be visualized as a leaking blood vessel complex under the retina. It is regarded as a safe test, but people should expect some yellowish skin discoloration and orange urine. Most people have no difficulty with this testing, although a low percentage of people will experience some nausea. Any angiogram test, however, can be associated with allergic or even more severe reactions, and therefore, this test is typically reserved for people in whom wet AMD is noted or suspected.
Optical Coherence Tomography (OCT) is a non-invasive, office-based imaging technique that uses low energy laser to scan the macula and determine whether there is fluid in the macula, potentially signifying wet AMD. It is a commonly used test as an adjunct to fluorescein angiography to help diagnose wet AMD. It can also be used to assess the response to treatment for wet AMD. OCT is performed with no risk to the patient.
Prognosis
Most people with AMD will retain good central vision and the ability to read in their lifetime. This is because 90% of people have dry AMD. This is associated with a more favorable prognosis. People with wet AMD will suffer central vision loss if left untreated. If it affects both eyes with associated vision loss, then the patient may progress to legal blindness, although AMD does not lead to total loss of vision. Thankfully, new treatments are improving the prognosis even for people with wet AMD.
Treatment
Dry AMD – There is no treatment yet to halt the progression or recover any vision loss from dry AMD. However, the Age Related Eye Disease Study (AREDS) demonstrated that a specific formulation of anti-oxidant vitamins and minerals can reduce the risk of progression of dry AMD to more advanced stages and associated vision loss. The components of the AREDS2 formula are as follows:
500 mg Vitamin C
400 IU Vitamin E
80 mg Zinc oxide
2 mg Copper oxide
10 mg Lutein
2 mg Zeaxanthin
It is important to check with your medical doctor before starting this AREDS2 supplement. In general, Vitamin E supplementation should not exceed 400 IU, and smokers should not be on any Beta-carotene supplementation due to an increased risk of lung cancer. There are AREDS formula vitamins available that do not have Beta-carotene that are appropriate for smokers. In fact, the AREDS2 formula has simplified this by replacing Beta-carotene with Lutein and Zeaxanthin. The AREDS2 formula is beneficial regardless of smoking status.
Based on epidemiologic studies, certain lifestyle and nutritional changes may be beneficial. Based on what is known to date, the following recommendations may be made in hopes of improving the prognosis of dry AMD:
- Stop smoking. Smoking has been associated with vision loss and more advanced forms of AMD.
- Eat a diet rich in colorful vegetables and fruits. These food groups have been associated with lower rates of progression to advanced AMD and contain anti-oxidants (eg. Luetin) which may slow progression of disease.
- Control blood pressure. High blood pressure is associated with more advanced AMD.
- Consider eating food rich in Omega 3 fatty acids. Omega 3 fatty acids are found in cold water fish such as tuna and salmon and are believed to be associated with less advanced AMD.
- Be physically active. People with AMD who are physically active several times a week may reduce their risk for progression to advanced AMD and vision loss.
Wet AMD – The prognosis for people with wet AMD is improving. There are more effective treatments now than was available just a few years ago but still no cures exist for AMD. The primary treatments are new drugs aimed at blocking growth factors.
Anti-Vascular Endothelial Growth Factor (VEGF) Agents:
The most recent treatment development for wet AMD was the FDA approval of Eylea (aflibercept) in 2012. Prior to this, Lucentis (ranibizumab) was FDA approved in 2006. This was the first treatment shown to improve vision in many people with wet AMD. Both Lucentis and Eylea are administered in the office by an intraocular injection and typically dosed monthly for the first few treatments. The eye is prepped with antiseptic solutions and topical anesthetic drops. The injection is very well tolerated being relatively painless and only rarely associated with any complications. Treatment may need to continue for up several years or more depending on the nature of the wet AMD and response to treatment, although the frequency and total number of injections may vary considerably among patients.
The risks of intraocular injections such as with Lucentis include hemorrhage, retinal tear, and infection, all of which are very rare. Anyone who receives an injection and subsequently has increased pain or loss of vision should contact their doctor immediately as these symptoms could indicate a serious infection.
Lucentis is a humanized antibody fragment that works by blocking an important growth factor of choroidal neovascularization called vascular endothelial growth factor (VEGF.) By blocking VEGF, both the growth and leakiness of the abnormal blood vessels is reduced. Studies with patients on a course of Lucentis showed that 70% of people on treatment will maintain or improve vision and 30% to 40% of people have relatively large degrees of visual improvement. However, there can still be vision loss despite ongoing Lucentis therapy.
Avastin (bevacizumab) is another drug used to treat wet AMD. Avastin is FDA-approved for use in people with certain types of cancer. Like Lucentis, Avastin is an antibody to VEGF. Retina specialists have been performing intraocular injections of Avastin, similar to Lucentis and Macugen (below), to treat wet AMD. This is considered off-label use of this medicine. However, there is considerable clinical experience and now published studies that indicate that Avastin is beneficial for people with wet AMD. The clinical impression of retina specialists is that Avastin is comparably safe and effective to Lucentis, but scientific data are less rigorous compared to the large FDA registration trials conducted with Lucentis. Any intraocular injection therapy, even when using only small doses in the eye, can potentially have side effects in the body, but, thus far, few (if any) side effects of Avastin have been recognized when used to treat AMD.
Macugen (pegaptanib) is a growth inhibiting drug that blocks VEGF to some degree and can also slow the growth of choroidal neovascularization and to reduce leakage in the macula. Macugen was the first approved intraocular injection therapy for wet AMD, but is generally considered to be less effective than Eylea, Lucentis, and Avastin.
Photodynamic therapy (PDT) with Visudyne (verteporfin) is another treatment for wet AMD. It utilizes an intravenous injection of a photosensitizing drug called verteporfin (Visudyne) and a non-thermal laser light to try and reduce leakage from certain types of choroidal neovascularization. It typically does not improve vision when used alone, however, it is being explored as an adjunctive agent to anti-VEGF therapy such as Lucentis or Avastin and to intraocular steroid therapy.
PDT is a timed, office-based procedure. The Visudyne drug is infused into the vein over 10 minutes and then allowed to collect within the choroidal neovascularization over another 5 minutes. The choroidal neovascularization is then exposed to a low energy laser light for about 90 seconds to activate the drug only within abnormal blood vessels in the macula. This produces a chemical reaction within these abnormal blood vessels to reduce blood flow and leakage. The treatment is often repeated at 3 month intervals.
Visudyne clears itself completely from the body over several days. The skin and eyes must be protected from sunlight with clothing and special sunglasses for 2 days after the treatment. No driving is allowed while wearing the sunglasses. Sometimes PDT is combined with other treatments such as Lucentis or with steroid injections to try and attack choroidal neovascularization from several different mechanisms of action.
Laser Photocoagulation
Thermal laser photocoagulation may be used in certain, rare cases of choroidal neovascularization where the abnormal blood vessels are not beneath the center of the macula. Thermal laser treatment attempts to heat and destroy choroidal neovascularization but also damages overlying vision cells to some degree. Accordingly, this procedure is typically considered only when the abnormal blood vessels are far from the center of the macula. A major problem with thermal laser treatment is recurrent choroidal neovascularization which can develop in 50-60% of people.
Miscellaneous Treatments
Low vision aides may help improve the quality of life for people whose vision is impaired to the point that they cannot carry out important visual activities of daily living such as reading mail or writing checks. Low vision rehabilitation involves using specific magnifying optical devices and lighting aids to assist in performing specific vision functions. Although low vision aids are no cure for AMD, they may be helpful in performing essential visual tasks. Low vision centers can also be a good resource for non-optical aids such as books on tape, large print reading materials, and writing guides.
